What is a reverse total shoulder replacement?
A reverse total shoulder replacement involves removing the damaged parts of the shoulder and replacing them with artificial parts.
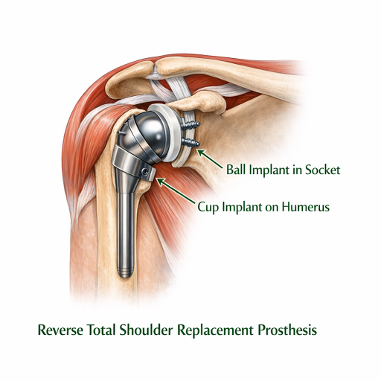
The difference between a reverse prosthesis and a standard shoulder replacement is that in a reverse prosthesis, the ball is placed on the socket side of the joint. This is opposite of where it is located in nature, or “reverse” of what you would expect. The socket is then placed on the arm side where it is supported by a metal stem in the arm bone (the humerus). In a standard surgery, the metal ball attaches to the upper part of the humerus and the new plastic socket attaches to the shoulder blade. This more closely follows a person’s real anatomy.
A reverse total shoulder replacement is a better option for people with certain injuries or conditions, as reversing the ball and socket arrangement of the joint changes the centre of rotation of the shoulder, which allows other muscles to compensate for a malfunctioning rotator cuff. These conditions include:
• Rotator cuff tear arthropathy: The most common reason to consider a reverse prosthesis is when there is arthritis of the shoulder joint and the rotator cuff tendons are torn or gone. A reverse prosthesis can significantly reduce pain and restore some range of motion in the shoulder.
• A previous standard shoulder replacement causing lingering symptoms: Healthcare providers may recommend reverse total shoulder replacement to people who have already had a standard shoulder replacement for osteoarthritis, fractures or other reasons. These people may still have symptoms, including pain and loss of motion, that a reverse total shoulder replacement could address. The surgery to place a reverse prosthesis after a standard shoulder replacement was performed is complicated. The existing shoulder prosthesis must be removed before the reverse prosthesis can be placed.
• Shoulder fractures: A person may need a reverse prosthesis for some fractures of the shoulder area, particularly those close to where the ball attaches to the shaft of the arm bone (humerus). In some cases, the bone is broken into many pieces or the ball may be split into parts.
The reverse prosthesis is good at providing pain relief. Studies from Europe indicate that about 85-90% of patients who have this procedure obtain excellent pain relief. The degree of pain relief depends largely on the reason for the procedure. The degree of pain relief for revision cases is lower than for first-time replacement, and this is believed to be due to the scar formation and long-term damage.
The reverse prosthesis should also restore some range of motion to the shoulder, but the degree of this improvement is not as predictable as pain relief. Most patients can reach the top of their heads without the need to tilt their head. Most patients also see improvement of motion in other directions. However, if the rotator cuff was torn completely, there may not be an improvement in the ability to reach out to the side away from the body (external rotation).
Like every surgery, reverse total shoulder replacement carries risk. These include:
• Dislocation of the artificial joint is the most common complication after a reverse total shoulder replacement. The humerus or arm portion (the socket) can become dislodged or disconnected from the ball (the shoulder blade part). This complication is more common with the reverse prosthesis than with regular shoulder replacements. Typically, it can be managed by placing the arm back into the proper place and immobilizing the arm for a period of time. If the prosthesis continues to dislocate then sometimes further surgery is needed to tighten things up.
• Infection occurs rarely but can be frustrating for the patient and physician alike. Sometimes the infection can be controlled by surgery to wash out the joint and with antibiotics. If the infection becomes chronic despite treatment, then there are options for solving the infection, but they largely involve further surgery.
• Excess blood loss. Most patients donate blood before the surgery, which can be given back to them if needed. Only about 10-20% of patients who are having a first-time joint replacement need a blood transfusion, compared to almost 80% of patients who have a revision surgery, which lasts longer.
• Damage to the surrounding nerves (which might impair arm movement). Tingling, numbness and weakness can occur if the nerves to the arm stretched during surgery.
• Break (fracture) of one of the shoulder bones
• Complications from anaesthesia or a reaction to certain drugs
• When the arm part of the prosthesis makes contact with the bone of the shoulder blade in certain positions, it can create a groove in the bone of the shoulder blade that usually is not painful. This complication does not typically require surgery and can be controlled by avoiding certain arm positions and with medication.
• Injury to blood vessels is very rare but can happen particularly when there is a lot of scaring, and the patient has had multiple operations.
• Other rare complications include:
• Blood clots in the legs (deep venous thrombosis) which can travel to the lungs (pulmonary embolus)
• Heart attacks
• Strokes
Recovery from a shoulder replacement takes time. On discharge from hospital the arm will be in a sling, with physiotherapy commencing 2-4 weeks following the procedure. Your activities will need to be modified, and you will be unable to drive for 6 weeks. Pain swelling and bruising can be common for several months following surgery, and it often takes 6-12 months to make a full recovery.